HIPAA Compliance Challenges in Home Health Agencies
The Health Insurance Portability and Accountability Act (HIPAA) was put into place to safeguard patient information from improper access, breaches, and misuse. Home health agencies (HHAs), though, have special challenges in sustaining HIPAA security compliance due to remote caregiving settings, mobile access to patient information, and changing cybersecurity threats.
While large health systems and hospitals spend a great deal of money on hospital cybersecurity companies and healthcare cybersecurity services, home health providers often run on minimal IT capabilities, becoming a prime target for healthcare cybersecurity threats.
The following article investigates the most frequent HIPAA compliance loopholes for home health and prescribes the solutions to cut cybersecurity risks for healthcare.
Understanding HIPAA Compliance in Home Healthcare
HIPAA compliance in home health environments is dictated by the HIPAA Security Rule, which stipulates the HIPAA security requirements for safeguarding electronic Protected Health Information (ePHI).
Principal HIPAA Rules That Impact Home Health Providers
- HIPAA Privacy Rule – Regulates the release of PHI and the protection of patient rights.
- HIPAA Security Rule – Mandates physical, administrative, and technical protections for ePHI.
- Breach Notification Rule – Requires reporting of security incidents to impacted patients and regulatory agencies.
- HIPAA Compliance IT Requirements – Addresses secure storage of data, access management, and HIPAA cybersecurity framework adoption.
Why HIPAA Compliance is a Significant Challenge for Home Health Providers
1. The Mobile & Remote Character of Home Health Work
Home health providers use mobile phones, remote connections, and cloud technology to provide care effectively. As opposed to hospitals, whose healthcare cybersecurity is concentrated, HHAs operate in dispersed settings, with caregivers retrieving PHI from remote points.
Numerous caregivers use their own personal smartphones, tablets, or laptops to record visits to patients, share information with colleagues, and prescribe medications. This raises exposure to unauthorized entry, hacking, and data capture, contravening HIPAA security requirements.
Key Risks
- Unencrypted patient data on personal devices.
- Lost or stolen devices with sensitive PHI.
- Lax network security at home (public Wi-Fi threats).
HIPAA Compliance Solutions:
- Enforce HIPAA network security requirements, such as encrypted storage and secure VPN access.
- Employ remote wipe features to erase PHI from lost or stolen devices.
- Limit personal device use and impose HIPAA security compliance using secure mobile apps.
2. Inadequate Data Encryption & Communication Security
Most HHAs are not compliant with HIPAA encryption standards, and patient information remains exposed when transmitted, stored, or accessed over the internet. Non-encryption is one of the main reasons for data breaches in home healthcare since cyber threats could intercept non-encrypted PHI with ease.
Common HIPAA Encryption Rule Violations:
- Using unencrypted emails to send PHI.
- Having unencrypted patient records saved on home computers or mobile devices.
- Utilizing messaging applications not HIPAA compliant for communication among caregivers.
HIPAA Compliance Solutions:
- Use end-to-end encryption to satisfy HIPAA data security requirements.
- Make the use of secure, HIPAA-compliant communication platforms mandatory.
- Encrypt data stored and data in transit to satisfy HIPAA cyber security requirements.
3. Weak Network Security & Unsecured Wi-Fi Connections
Most home health caregivers use insecure Wi-Fi networks at patients' homes, coffee shops, or public spaces when accessing patients' data. Most HHAs lack stringent network security policies, making them prone to man-in-the-middle attacks, unauthorized access, and data breaches.
Important Network Security Risks in Home Health:
- Unsecured public Wi-Fi used by caregivers while working.
- Home routers with inadequate security settings are exposing patients' data.
- Firewalls, intrusion detection systems, and VPNs not available.
HIPAA Compliance Solutions:
- Institute HIPAA compliance network security policies that mandate that all remote access must be done via secure VPNs.
- Mandate caregivers to only use secure, private Wi-Fi connections.
- Regular cybersecurity audits to detect network vulnerabilities in accordance with HIPAA technology requirements.
4. Inadequate Multi-Factor Authentication (MFA) & Access Controls
Most home health agencies fail to implement MFA, making systems susceptible to unauthorized access, phishing, and credential theft. In the absence of adequate access control measures, PHI can be accessed by unauthorized staff, resulting in HIPAA violations.
Typical Access Control Failures in Home Health:
- Caregivers exchanging login credentials for convenience.
- Weak passwords that are easily guessable.
- Lack of role-based access control (RBAC) to restrict access to sensitive information.
HIPAA Compliance Solutions:
- Apply MFA to all systems storing or accessing PHI.
- Apply RBAC policies so that only authorized personnel can access PHI.
- Apply password managers to enforce strong password policies as per HIPAA compliance IT security guidelines.
5. Failure to Perform Regular HIPAA Risk Assessments & Security Audits
Most home health providers do not perform periodic HIPAA risk assessments, and thus security vulnerabilities are not detected until a breach has taken place. Disregarding security audits is a clear contravention of HIPAA cybersecurity requirements.
Critical Risks of Forgoing Risk Assessments:
- Unidentified vulnerabilities resulting in data breaches.
- Increased penalties for HIPAA non-compliance upon audit.
- No incident response planning, enhancing breach impact.
HIPAA Compliance Solutions:
- Perform annual HIPAA risk assessments as mandated by HIPAA compliance regulations.
- Recruit third-party cybersecurity auditors to conduct independent security reviews.
- Develop a Breach Response Plan to address security breaches effectively.
6. Insufficient Employee Training & Cybersecurity Awareness
A primary HIPAA compliance deficit for home health is the lack of employee training. Administrative staff, nurses, and caregivers usually don't know the HIPAA security rules and, as a result, fall victim to phishing schemes, social engineering tactics, and inadvertent disclosures of PHI.
Typical Training Gaps
- Staff members getting duped by phishing attacks, revealing patient information.
- Failure to identify cybersecurity risks in everyday processes.
- Unawareness of HIPAA privacy and security regulations.
HIPAA Compliance Solutions:
- Provide regular HIPAA cybersecurity training to all staff members.
- Conduct simulated phishing attacks to gauge staff awareness.
- Make annual compliance certification mandatory to enforce HIPAA security policies.
Legal & Financial Consequences of HIPAA Non-Compliance
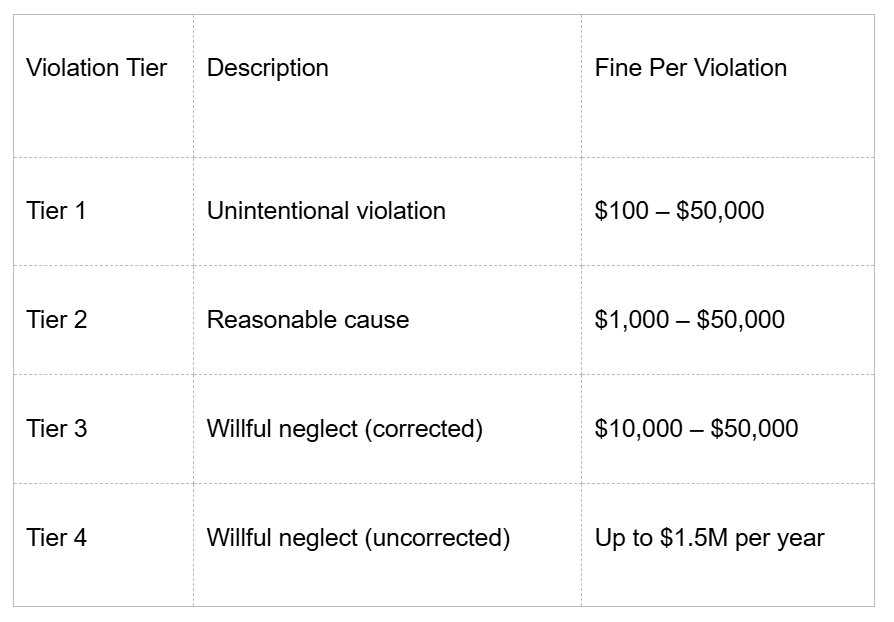
Home health HIPAA violations have severe legal and financial consequences. The Office for Civil Rights (OCR) strictly enforces HIPAA security regulations and, in the case of non-compliance, expects hefty fines, lawsuits, and damage to reputation.
1. HIPAA Violation Tiers & Penalties
HIPAA violations are classified into four penalty tiers with increasing fines depending on the severity of non-compliance.
HIPAA Compliance Action Plan for Home Health Agencies
To achieve HIPAA cybersecurity requirements, home health providers ought to follow the below 6-step compliance plan.
By following this HIPAA compliance framework, home health agencies can reduce security risks and protect patient trust.
Final Thoughts
HIPAA compliance is non-negotiable for home health providers. By addressing network security gaps, encryption vulnerabilities, and staff training deficiencies, agencies can prevent data breaches, penalties, and reputational harm.
Take the next step in securing PHI and ensuring HIPAA security compliance by partnering with Gini for expert cybersecurity solutions.